Systems dynamics as an interactive patient education tool for
preventing coronary artery disease and myocardial infarction
Lewis Mehl-Madrona, MD, PhD
Native American Research and Training Center
Department of Family and Community Medicine
University of Arizona School of Medicine
1642 E. Helen St.
Tucson, AZ 85719, U.S.A.
Voice: 01-520-621-5075
Fax: 01-520-621-9802
E-mail: mmadrona@aol.com
Introduction:† Being able to predict when a person would have
a myocardial infarction (MI) would have multiple implications: (1) that we
understand what leads to MIís, (2) that we have a means to identify patients
who are at risk for having immanent MIís and that we could help them to delay
or avoid an MI, and (3) that we could give patients accurate feedback about the
results for them of risk factor modification.†
The goal of this research was to develop a systems dynamics computer
simulation model that would predict MIís.
Methods: †††††† A model created to simulate the course of patientsí
cardiovascular health and disease, beginning at birth and predicting time in
months at which eventual coronary artery occlusion and myocardial infarction
(MI) would occur.† The model was developed
on a cohort of patients with acute myocardial infarction using such variables
as cholesterol; systolic and diastolic blood pressure; sex; menstrual status;
triglyceride levels; HDL and LDL cholesterol levels; glucose levels; family
history of age at initial myocardial infarction; smoking status and amount;
exercise frequency, duration, and intensity; activity level of the patientís
lifestyle; amount of dietary fat consumed; weight and height; hostility; levels
of psychosocial stress; and a number of other variables known to influence the
rate of development of coronary artery disease.†
Psychosocial data was obtained about stress, support and
depression.†† Lifestyle data was obtained
about exercise, activity levels, diet, alcohol, caffeine, cigarettes and drug
consumption.†
A second group
of patients interacted with the model to study how patients would react to the
feedback provided and whether or not they would change risk factors.† Patients were given specific predictions with
graphs about when they would be expected to have a heart attack and predictions
of how much longer we would expect them to live with risk factor
modification.† They were permitted to
query the computer regarding how other changes they might make would affect
their longevity.† For example, patients
could stop smoking and begin exercising at the present time, re-run the
simulation, and determine how this behavior change in the present would affect
the time before they could expect to have a myocardial infarction (heart
attack; crise cardiac).† Patients could “bargain”
with the simulation to determine what combination of risk factors they were
willing to change to obtain specific lengthening of time before they could
expect a myocardial infarction.
Results:
Sample characteristics.† Of the 44 patients used for the initial validation
testing, 14 were women and 11 were Hispanic.†
Systolic blood pressures ranged from 79 to 176 (mode = 130).† Diastolic pressures ranged from 44 to 110
(mode = 80).† Cholesterol ranged from 118
mgm/dl to 373 mgm/dl (mode
= 222 mgm/dl).†
Triglycerides ranged from 56 mgm/dl to 710 mgm/dl (mode = 139 mgm/dl).† Random blood glucoses ranges from 80 mgm/dl to 724 mgm/dl (mode = 132 mgm/dl).† Activity
levels ranged from 0 to 6 (mode = 0).†
Total CK levels ranged from 102 to 6200 I.U. (mode = 712 I.U.).† Time of initial myocardial infarction ranged
from 432 months to 989 months (mode = 635 months).† Pack years of smoking ranged from 0 to 210
(mode of 0).† Body mass index ranged from
0.0127 to 0.0483 (mode = 0.0254).† Table
2 shows the breakdown in MI Outcome Index by race.
Comparisons to conventional statistics.
1.† Cluster analysis.† Both the Joins and the K-means procedures
were used.† Despite attempting all
possible permutations of variables, the best classification obtained was 13
correct assignments out of the 22 test cases (59.1% accuracy).† This was achieved by using all independent
variables with the single linkage method (nearest neighbor).† The distance metric was the Pearson
correlation coefficient.† This compares
to 88% correct classification with dynamic systems modeling.
2.† Multiple regression analysis.† A multiple regression model predicted 26.6%
of the variance (p = 0.018).† A
borderline significant interaction of race and sex was noted with white males
faring the worst.† The most significant
and best predictors were triglyceride and cholesterol levels.
Dynamic Systems Modeling.† The model correctly classified 88% of
patients.† The false positive rate was 6%
and the false negative rate was 13%.† The
false positive patients included a 64 year old Hispanic female with a blood glucose of 529 mgm/dl,
cholesterol of 373 mgm/dl and triglycerides of 323 mgm/dl.† The
assumption of 20 years of chronicity may not have been accurate for this
patient or she may have had an unmeasured protective factor operable.† The first false negative was a 43 year old
white, post-menopausal female with all normal indicators except for 25
pack-years of cigarette smoking.† The
second false negative was a 42 year old Hispanic male with all normal
indicators except for a blood pressure of 155/105 and a cholesterol level of 234 mgm/dl.
An unidentified
risk factor was isolated in the learning sample and on closer inspection was
found to be family history of early MI.† It
became prominent when age was greater than 57 years, blood pressure normal,
smoking less than 2 packs per day, body mass index greater than 0.0177 and
cholesterol levels between 166 and 239 mgm/dl,
with glucose levels between 100 and 210 mgm/dl and
triglycerides between 105 and 185 mgm/dl for
men.† When these parameters were
exceeded, the genetic effects appeared to be sufficiently overshadowed as to be
rendered non-operable.† It was operable
in women with a positive history when age was greater than 5o, blood pressure
normal, non-smoking was true, race was white and cholesterol was greater than 200 mgm/dl with all other indices
normal.
Results of
Interaction with the Model:† 21
patients who interacted with the model were followed for an average of 5.9 mos.
(range 5 to 20 mo).† The patients were seen at 4-8 week intervals
to update data and to interact with the model.†
Nineteen reduced some aspect of risk behavior; 19 increased exercise
and/or activity (90%); 4 increased HDL cholesterol (21%); 8 decreased LDL
cholesterol (38%); 12 decreased BP (58%). Patientsí acceptance of the systems
dynamics model was high.† They preferred
what they learned from the model to the standard of medical care, which
consists of lectures from the physician to change behavior (“stop
smoking, lose weight, exercise) or else.†
In the standard medical approach, “or else” is poorly specified and patients can question whether
or not the information presented applies to them or not.† Patients being able to use the systems
dynamics model to evaluate their own personal risks and benefits and make
choices based upon data presented rather than the usual lecture approach of
their physician.
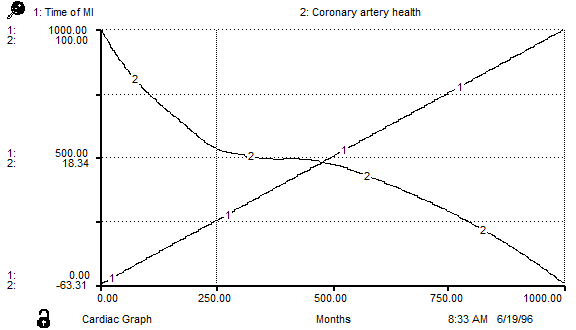
Sample
Output.† Figure 1 shows the
prediction for a patient with many risk factors.† The time (in months) at which line 1 (Time of
MI) changes slope represents the time at which an MI is predicted to occur
(about 520 months or age 43 and 4 months).†
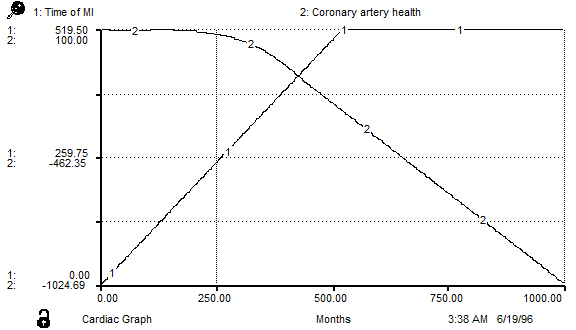
Figure 2 shows
the graph for a patient with no risk factors and for whom no MI is predicted at
even 1,000 months (age 83).†